
This essay offers a new explanatory framework and treatment vista by using silicone cupping vessels to remodel discordant fascia. The flexibility and maneuverability of these instruments smooths the way for these possibilities. My aim is to give a modern take on what has been found to work especially well for people suffering from chronic soft tissue injury and restricted mobility. A focus will be to explain the therapeutic mechanism that appears to take place within the local subcutaneous tissue underneath an active cupping vessel. My speculations also add to the current wave of interest associating the pathways of the fascia throughout the body with the regular TCM meridians and the jingjin, variously known as muscle or tendino-muscular channels. I consider this cupping adaptation to have far reaching potential.
Qualitative methodology
Quantitative scientific research on what happens to the local tissue affected by a vacuum has so far been unable to determine this proposition. Our assertions therefore are based on qualitative clinical examination and trial procedures (a). Where we suspect the fascia, also known as connective tissue, may be implicated, palpatory examination has regularly revealed discordant subcutaneous tissue structure at those corresponding locations. After treatment, we have noted a significant change in the structural integrity of the same area. In response, patients consistently report feeling less pain and freer movement. Because fascial disorders surrounding the hip area have responded so well to treatment, and because it is such a common and debilitating problem, my clinical discussions will mostly involve this region.
In the classes we teach, when time comes for instruction concerning hip pain, we have adopted the following protocol before students have the opportunity to practise on each other. First, we establish if someone in the group suffers a hip injury or discomfort and is willing to participate in the demonstration. It is such a common issue that we usually have to decide who is most in need.
Second, we palpate the general region to find if and where the tissue structure is errant. We have consistently noted that patients confirm that the area in which we diagnose disarray of the fascia is indeed their subjective site(s) of pain.
Third, students are invited to palpate the same area to see if they too can feel and distinguish between indurations, fibrous tissue patterns and other fascial disorders, and compare that with other zones where the tissue is regular and free from discomfort.
Fourth, we proceed with treatment. Fifth, students follow up and re-examine the tissue. Unswervingly it is agreed that the change is impressive. We then ask the person who has been treated to walk around, stretch, and generally get a handle on how they feel.
Most importantly so far, in both clinic and in class, we have not had a case where the feedback has been other than very positive. It has even been common for people to experience joy at how pain-free they feel and how well they can move. Follow-up communications indicate that the results are long lasting.
We suggest also that the remodelling of the superficial fascia, and the release of the associated muscle tissue beneath, has a trickle-down effect to influence the fascial weave within the internal organs. Research into the interplay and the interactive mechanisms of the fascia, and the importance that it has on physiological function, is pointing in such a direction. Of course traditional Chinese medical theory has proposed the surface affecting the inside dynamic for a very long time.
Flexible cupping vessels
For almost 20 years, I have trialed flexible cupping instruments. However, it has been close to the past six years that, together with colleague Shirley Gabriel, we have discovered a new direction for cupping, which to the best of our knowledge has never been engaged before.
We arrived at these practices by first applying flexible cupping instruments to regions of the body that were either difficult or impossible to treat with traditional solid instruments.
We then realised, through trial and error, that by sliding a flexible cup very, very slowly (“at snail’s pace”) over knotted and/ or congested fibrous tissue hampered by injury, pain and immobility, the palpable subcutaneous tissue directly below the cup was quickly remodeled.
We also discovered that the local effect was amplified by sliding a cup very slowly along a distal margin of a TCM channel linked with the focal site of treatment. In a parallel mapping discourse of the body as an integrated system where distal regions can affect local disharmony, Thomas Myers (2010) recommends treating local fascial dysfunction by engaging the far away geography of corresponding fascial pathways, which he calls “myofascial meridians” in his “anatomy trains” system.
On the heels of our initial experiences, we began studying the literature pertaining to the fascia and found a substantial theoretical basis for our own practical findings. We came to realise, in what we still relish to be a fortuitous “synergy in time”, that there is an active group of researchers and therapists with whom we share a camaraderie of ideas. I speak of those pioneers and their contemporaries who propose a new purpose and direction for the fascia, based on ideas and findings that have otherwise met with little interest from mainstream medical opinion and research.
What Shirley and I were especially interested in however were the therapeutic ramifications that cupping had on the fascia. Those we cite throughout this essay are much appreciated for their knowledge and insight into this physical mechanism that appears to respond so well to cupping.
“We realised that by sliding a flexible cup very, very slowly over knotted or congested fibrous tissue that the palpable subcutaneous tissue directly below the cup was quickly remodeled.”
Modern Cupping
We have also been occupied in developing other initiatives and treatment strategies for cupping besides myofascial therapy. For decades, I have applied cupping with excellent success in relieving pain and restoring integrity to other soft-tissue disorders. This includes treating scar tissue, reducing stretch marks and clearing cellulite. More recently we have adopted flexible cups to more effectively disperse trigger points, as well as using other new cupping instruments such as miniature hand-blown glass cups with an attached aspirator pump applied at local points to clear sinus congestion, significantly reduce and often completely clear up inflammatory skin conditions, ease TMJ syndrome and relieve mild headache. Combined together with additional practices, we have coined the term “modern cupping” to describe this broad spectrum of cupping possibilities that may come to be recognised as Phase 3 in cupping’s long therapeutic career.
“Modern cupping simply adds to the therapeutic range of cupping. It is but one set of important practices within a large therapeutic context.”
The term Phase 3, and its connections with “modern cupping”, are by no means meant to imply that “pre-modern” ideas, instruments, methods or practices are in any way obsolete or anachronistic. Nothing could be further from our intention. They are vital therapeutic legacies that deal most effectively with the broad range of treatments that are best served by traditional rationale and apparatus.

Fig 1: Australia aboriginal medicine man sucking to withdraw evil magic (Batty, Allen and Morton, 2005:159)
A basic theoretical premise for our work is recognising that tools in themselves define a task. For instance, a spade serves us best when digging a hole. So too, all the many transcultural cupping practices that are “traditional”, being based on pre-biomedical explanations about why we get sick or suffer pain, are best performed by traditional tools and methods of application. Modern cupping simply adds to the therapeutic range of cupping. It is but one set of important practices within a large therapeutic context.
I also purposefully use the term “phase” to denote a period or concept that is not separate or bound by sharp parameters, because phases interact and can mutually benefit one another. For example, in practice I frequently combine traditional and modern cupping. Only recently during a class in Seattle, I treated a student who had a chronic hip complaint. By palpation, I discovered a depression in the musculature that was clearly cold and deficient. I also found a proliferation of tense spider web-like fascial disorder surrounding her greater trochanter. First, I used the glass and flame method to draw out the coldness, and then tonified the deficiency, using the methods described in an essay previously published in The Lantern (“Cupping Deficiency”, 2011). Second, I employed a flexible silicone cup to knit and restore integrity to the fascia. Third, I applied the sliding or moving cup method with a silicone cup along the lower limb pathway of the Gallbladder meridian. From an “anatomy trains” perspective this line going down the middle lateral surface of the leg connecting with the hip is known as the “lateral line”. Despite time constraints in class making it possible to give her only a demonstration treatment, she reported in an email one month later a significant and lasting improvement.
I will now frame our proposal within an historical context based on our definition of cupping to be vacuum applied at the skin surface for a therapeutic effect. History and the present are a two-way time machine that presents a fascinating insight into many healing essentials. What we understand about cupping today allows us also to reach back in time and reconnect with our primal selves.
Phase 1 and Phase 2 of cupping
It has been established over a vast stretch of time that the effect of applying vacuum to the skin surface is effective in dealing with many illnesses and pain syndromes. Cupping has proved to have a remarkable ability to be interpreted transculturally and adopted into different medical paradigms, since it began at its most basic and instinctive as oral suction to draw out stings, toxins and other irritations. In my opinion, prior to Modern Cupping, there have been two other significant and ongoing phases of cupping practice.
Phase 1 belongs within humankind’s first complex medical tradition, known as either supernaturalistic or shamanic curing. In this tradititon, which goes back into the mists of time, the mysteries of illness, suffering and unexplainable death are attributed to malevolent other-worldly influences, such as spirits, ghosts, disgruntled ancestors or alternatively the infliction of an extraordinary power such as the evil eye. It is the shaman, the person endowed with the power and special skills required to mediate between these forces, who carries out treatment and brings about a cure. Besides ceremonies of conciliation, the most important physical intervention performed upon the patient is sucking at the skin surface to withdraw whatever harmful intrusion has made its way inside the body or soul. Mircea Eliade (1989: 256), a professor of the history of religion and renowned scholar of shamanism, described suction as “a classic method of cure”, and A.P. Elkin (1994: 41) in his revered book written during the 1930s titled Aboriginal Men of High Degree refers to sucking as “the means by which the doctor exercises his magical and psychic power and extracts and casts away the badness”. Consider as well that supernaturalistic healing continues to be embraced throughout many regions of the world to this day, and one can readily comprehend the role of vacuum throughout the millennia as being monumental.
Phase 2 of cupping is founded on its use and ability to treat pain and suffering brought about by natural, in contrast to supernatural, causes. Naturalistic etiologies for illness, such as disharmony of the body’s elements or the penetration of climatic factors, became some of the clinical reasons for its adoption. We also find that cupping vessels largely replace oral suction, making it possible to maintain a vacuum for an extended period of time, as well as being far more sanitary.
Based on reliable historical evidence, Phase 2 began during the late 6th century or early 5th century BC in Greece, but I have more than a sneaking suspicion, yet to be confirmed, that it was probably engaged much earlier in Egyptian, Assyrian or Minoan medical ministrations, for example. On a carved relief, two cupping vessels can be clearly identified suspended between the heads of the seated physician and his standing patient (or student). As the visual record from around this time often indicates, such importance and authority was given to the cupping vessel that, along with the staff, it symbolised and identified a physician, just as the stethoscope identifies the biomedical doctor today.
The first textual reference to cupping came a little later, engraved on an iamata or marble tablet at a sanctuary dedicated to Asklepios, the god of healing, at Lebena, Crete (Christpoulou-Aletra and Papavramidou 2008: 899). However, by around the middle of the 5th century BC, cupping had reached a hitherto unparalleled level of significance and application in the works of Hippocrates and his followers. Known collectively as the Hippocratic Corpus, these 60-odd (depending on how they are divided up) volumes, which have had the good fortune to survive, recommend cupping for many complaints including readjusting spinal misalignments, found in On Joints (Withington, 1968: 305), for staunching excessive menstruation, found in Aphorisms (Jones 1967:171) and in Epidemics (Smith 1994: 87), for uterine prolapse and for painful ear in Epidemics (Smith 1994:87), and for sciatica in Places in Man (Potter 1995: 63).
According to the Hippocratic writers, two important features maximised the therapeutic action of cupping. The first was the ideal shape of the cup, which was probably borrowed later by the Chinese because the shape of the regular Chinese glass cup nowadays is virtually identical. Second was the use of a flame, not only to facilitate a vacuum but also to bestow heat and enhance a cup’s drawing capacity to attract coldness and take it out of the body, or to redistribute the humours (fluids) and bring the body to balance. In tandem, the cup and heat represented a potent combination of forces that empowered the law of attraction, an early scientific theory that fascinated not only practising physicians performing cupping, but also the likes of Plato and Aristotle.

Fig 2: Late 6th or early 5th century BC tombstone showing a physician and his patient or student. The physician is seated on a folding stool holding his staff and stroking his beard; the boy (much restored) carries an aryballos of oil or, as Wickkiser (2008:16) interprets, hanging cupping vessels. Two cups are shown between the figures. Such cups were made of bronze, and after being heated were applied either to divert humours away from a site or attract them to it. (Phillips, Plate 8,1973)

Fig 3: The tombstone of Jason, an Athenian physician of the early 2nd century AD, depicts him examining a boy who appears to be undernourished. The object to the right is an enlarged cupping vessel which shows the importance given to the instrument and practice. (Phillips, Plate 9, 1973)
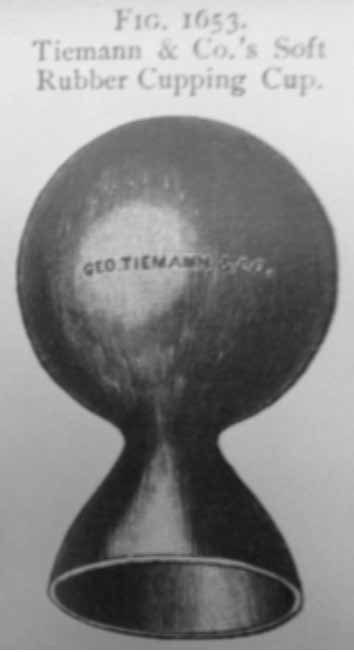
Fig 4: Tiemann & Co.’s “Soft Rubber Cupping Cup” featured in a bound catalogue of surgical instruments for sale.

Fig 5: An India rubber cupping vessel manufactured by Evans & Wormull in Illustrated Catalogue of Surgical Instruments, Apparatus and Appliances, 1893.
The therapeutic utilities of cupping were also successfully established within all of the world’s other great traditional and largely empiric medical systems, being traditional Chinese medicine (a hollow horn as a cupping instrument was first mentioned in the Ma Wang Dui medical manuscripts around 168 BC), the Ayurveda, Unani medicine (practised mostly in Asian Moslem communities and based on Hippocratic writings), Siddha medicine (originating in Southern India) and Islamic medicine. Cupping also continued throughout many parts of the world as a popular folk practice passed down from generation to generation (b). Indeed biomedicine is the only medical system to have essentially rejected cupping, which, as I have argued in Cupping as Therapeutic Technology (1996) was more to do with a lack of “fit” with the new paradigm of healing and practice rather than any lack of efficacy.
Phase 3: Historical precursors
Glass cups with an attached aspirator pump which is squeezed to create a vacuum probably followed shortly after the development of rubber bulbs in Europe somewhere around the mid to late 1700s. In a short essay published in the British Medical Journal, Underwood (1955:42) suggests that these were adapted for medical purposes following news brought back by the Portuguese of Amazonian natives using the latex sourced from local rubber plants to make bulbs, which they attached to tubes to perform enemas.
It was not until 1843 however, when Charles Goodyear invented the vulcanisation process that permitted rubber to be b. Readers may be interested to know that I have contributed a chapter to the coming third edition of Ilkay Chirali’s book Chinese Cupping Therapy with an essay called “Cupping’s folk heritage: people in practice.” manufactured and maintain its elasticity, that it was successfully incorporated into the make-up of cupping instruments. In their study on the collection of antique bloodletting instruments housed at the National Museum of History and Technology in Washington DC, Davis and Appel (1979: 28) believe that “the most significant innovation in cups came with the manufacture of cups of vulcanised rubber in the 1840s. Rubber cups could be easily exhausted without the need of a torch, and they were far cheaper and easier to manipulate than cups attached to a pump”. They also found that most medical catalogues of the late 19th century offered both all-rubber cups and glass cups to which a rubber bulb was attached. They surmise that “the appearance of these cups in all surgical catalogs indicates that they were widely sold”.
Other sets of cups were also available with a rubber rim around the lip to allow the cup to adhere comfortably against the skin, as well as help prevent air from entering inside and breaking the seal. Museum collections nowadays may contain only a few rubber cups (I haven’t seen any) because 19th century rubber typically deteriorated with time.
A couple of decades later in 1866, Samuel Gross (1866: 465), an American surgeon, considered the glass cup with a vulcanised rubber bulb to be the “most elegant and convenient contrivance, by far”((at least in relation to his practice of extracting blood by wet cupping). He went on, “In order to apply it, all that is necessary is to indent the top with the finger, the removal of which permits the part instantly to regain its former position, thus exhausting the air within, as it does with great force and efficiency.”
The first journal inclusion I have discovered to suggest a complete flexible cup is gleaned from the British medical journal The Lancet (1853: 255). In a correspondence to the editor, Thomas Stratton, a physician from Edinburgh, wrote Proposal to Substitute an Elastic Cup for the Present Cupping-Glass praising the inventor of the “atmospheric breast pump” made of a galvanised India rubber globe and suggested that “instead of the present plan of using the spirit-lamp or spirits of wine before applying the cuppingglass, would it not be much simpler and better to have cups made of the same substantial and elastic material, which answers so well when applied to the breast [to promote the flow of milk]?”
Early days
The medical technologies devised during any given era are a determinative influence on innovative modes of treatment. I first set eyes on flexible cups in the store at the Shanghai Hospital of Traditional Chinese Medicine in 1996. Blue rubber cups came snugly concertinaed in sets of four sizes. I purchased a couple of sets, brought them back to Australia and tried them out. They were made of a rigid rubber however, and because I was already a fan of the glass and flame method and appreciated traditional tools (glass and flame) for traditional applications, they never replaced my regular work over points and channels. However one application that impressed me greatly, which meant they were much more than a novelty, was placing them in situ while mobilising a satellite joint structure. This was indeed a boon in practice and brought tremendous results. As well, when I was pushed for time and couldn’t make a flour and water damper to set as a base over bony areas like the knees, or over protuberances such as the acromion process or the olecranon, the rubber cups proved to be effective.
Around six years later I was introduced to a newer rubber set from China. This incarnation was easier to manipulate and apply. As a matter of convenience on occasions in practice, I would slide them along the Bladder channel, or apply and then release them in quick succession throughout the back as a flash cupping method to relax the surface. One advance was obvious; they were easier to slide over uneven and difficult to maneuver surfaces of the body. However, one downfall of such rubber cups was their strong petro-chemical odour and the fact that after using them, the practitioner was required to thoroughly scrub off this lingering smell and bitter tasting residue. In addition, in time they did fray, especially around the lip. They were nevertheless, bless them, the tools that enabled Shirley and I to begin our work in applying them for myofascial release and for the dissolution of trigger points. This study will be presented a little later.
A few years later came a further manufacturing coup: replacing rubber with silicone. There are now many shapes and designs of silicone cups on the market, however those we recommend are made in China and available as three options. One set of four is coloured aqua, while the other comes close to being transparent. I have been made aware of a third type only recently in an email from the manufacturer. These are a set of transparent aqua cups. All are described as being “food safe”, have no odour, are durable and significantly softer, making them easy to apply. From large (1) to small (4), their measurements are:
- Large: 6.5cm diameter, 7cm height
- Medium: 5cm diameter, 5.5cm height
- Small: 4cm diameter, 4.5cm height
- Tiny: 3cm diameter, 3.5cm height
Along with each set comes a booklet of instructions. However these recommendations are simply suggestions to substitute them for traditional applications over acupuncture points or use them as convenient flame-free instruments for other Chinese practices such as sliding along meridians or for flash cupping. The following list of benefits and applications is based on how we relate to flexible cups for myofascial release, which we believe to be the great innovation for these new tools.

Fig 6: Rubber cup set.

Fig 7: A clear silicone cupping set.
Advantages of flexible silicone cups
While the glass and flame method is a timehonoured mode of practice, and a must for any well-rounded cupping therapist, the non-flame flexible instruments offer a range of different returns compared to their hardbodied (including vacuum pump) relatives. The following are some advantages.
Benefits for the practitioner
- A flexible cup feels more like a natural extension of the hand.
- Less concern about the lip losing contact with the skin surface.
- Permits a reverberation within the cup chamber for a far more sensitive “read” of the tissue. On occasions during the sliding cup procedure these vessels can transmit diagnostic indications of soft tissue dysfunction into the operator’s hand.
- Their shape can be changed and adjusted in the same way as the hand can change its shape or intention to perform different therapeutic procedures.
- Instantaneous application, especially when the momentum of the treatment is important.
- Allows the practitioner to rest the hands from repetitive and demanding effort and to get deeper into the soft tissue.
- Their flexibility and size permits almost any space to be cupped. They can be squeezed and configured into an oblong shape to complement a thin margin of tissue such as the upper fibres of the trapezius or between the lateral/medial malleolus and the achilles tendon, between the metatarsals and over the knuckles.
- Greater success in adhering cups (either stationary or sliding) on thin people.
- Can be used with ease as a self-help therapy; for example throughout the shoulders, arms and hands to release aches and pains caused by repetitive movements and overwork.
- Can be safely used in a confined space.
- Use does not compromise any property insurance rules or professional practice limitations, or any other safe conduct concerns from landlords and the like.



Fig 8, 9 and 10: The progress of two cups performing a myofascial release.
Benefits for the patient
- Makes it comfortable to receive myofascial stretching procedures.
- Eliminates any fear of flame.
- With the right instruction can be applied safely at home.
- They can be heated by immersing them in piping hot water
- Flexible cups are able to perform the entire range of treatment options, i.e. from gentle to deep and robust treatments.
General operating benefits
- Can be boiled to reduce micro-organisms.
- Compact and unbreakable; portability.
- Can be applied over tight areas before a practitioner adopts a yoga posture. A cup can even remain stationary during a stretch if practicable (Note: Shirley has developed a wide-ranging field of opportunity for this practice).
- On occasion can facilitate audible “popping” or “clicking” sounds from fascial tightness, which we interpret to be the emancipation of small nodules of pent up energy. This aids in easing tension and sharp pain. It is a fascinating phenomenon that I have not heard of before in any soft tissue forum.
- Can release tricky areas to apply other sorts of cups, such as the occipital (nuchal) line. Even feels great (stationary or being moved) on a follicly challenged scalp!


Fig 11: Being able to mould a flexible cupping vessel into the shape and purpose of the hand, the stretching of the superficial tissue and the drawing power of the cup are all highlighted in this photograph. Note the anchor hand stabilising the body, and the cup’s rim close to the fingers being moderately inverted into the soft tissue margin lateral to the greater trochanter to release the griping pain and contracture often found here. This appears far more fierce than it actually feels (it was described by the recipient as comfortable). Looking through a Chinese lens, we can see clear diagnostic information and a positive prognosis for weakened tissue structure (stretch marks) and the lingering pathogenic factors drawn to the surface. The general show of redness indicates an increase in local blood circulation. The stretch marks, which prior to treatment were cold and alabaster white, indicating weakness and poor circulation, are now mauve/purple, which demonstrates a deep blockage of cold and blood stagnation within the underlying tissue, until now. This colour will fade over two to three days and result in a healthier skin tone and stronger tissue structure. The small red blotch emerging on the right does by the end of treatment become a black spot with some elevation beyond the regular skin level. This shows the presence of a sharp, painful site of blood stasis, formed as a clot, thus the elevation, drawn to the surface. Lastly, some small red dots called sha, as in gua sha, appear.a They are fresh red and represent a recent issue.
The fascia
In a recent book titled Fascia: The Tensional Network of the Human Body, the fascia at its most uncomplicated is defined as being “the soft tissue component of the connective tissue system that permeates the body” (Schleip, Findley Chaitow and Huijing (2012: xvii). Levin and Martin (2012) also put it nicely by describing it as “the fabric of the body; not the vestments covering the corpus, but the warp and weft of the material. The other tissues, muscle and bone, liver and lung, gut and urinary, brain and endocrine, are embroidered into the fascial fabric.”
The fascia is so much more than what I noticed as a kid looking into a butcher shop window at the white sinewy stuff that wrapped around a cut of meat. Things didn’t get that much more exciting or sophisticated either in the anatomy classes I took decades ago. Times change and now we can wonder at all its structural and physiological intricacies, and at the multifarious roles it plays throughout the body, front to back, top to bottom, out and in. I think Thomas Myers (2010:41) sets the stage for its engagement, and for the required shift away from the tired compartmentalised approach to anatomy and medicine beautifully with: “The truth is the body is not assembled like a machine, but grown like a plant from a single seed spinning a single manifold membrane. This image of the body as machine is a limited one and blinds us to the synergistic aspects of whole-system functioning.”
“The truth is the body is not assembled like a machine, but grown like a plant from a single seed spinning a single manifold membrane.”
– Thomas Myers
One opportunity to survey the actual proliferation of the fascia throughout the body that had previously gone either unnoticed or ignored by the science of dissection has been to approach the body from a decidedly different angle. To achieve this has meant that instead of vertically cutting 90 degrees into the body, which emphasises the big structures, the slant is changed to finely carve across the body in horizontal planes, like a slicer cutting through sausage at a delicatessen. This has revealed the exquisitely fine sheaths of fascia that literally hold the body together from the surface to the inner depths. The osteopath Vince Paoletti (2006:168) further explains, “There is not a single part of the body that is not invested by some kind of fascial element. The study of anatomy demonstrates that the human body is constituted of large envelopes that enclose more or less extensive regions. Within these major compartments there are additional fasciae to enclose ever finer substructures without, however, creating any kind of discontinuity.”
“From a cupping perspective, powerfully drawing the blood to a site of fascial distress fulfills a crucial requirement for fascial rehabilitation.”
Historically, one has to look hard for likely descriptions of the fascia. Up until the 18th century in the West, according to Langevin and Huijing (2009), fascia was simply described as being a band-like material. In China, from as early as the Han dynasty (200 BC to 200 AD) there was intrigue about “the space between the skin and the muscles”., and in the Islamic medical tradition, Hunayn ibn Ishaq al Ibadi (809–877 AD), curiously renamed in most Western medical histories as Joannitius, described the composition of the “members” as “the bones, and the cartilages, and the membranes, which lie between the skin and the flesh”. (in Grant (ed) 1974:706). Sounds like it could be fascia.
The first great champion for the fascia was Andrew Taylor Still, the founder of osteopathy. Over a century ago he declared, “I know of no part of the body that equals fascia as a hunting ground. I believe that more rich golden thought will appear to the mind’s eye as the study of the fascia is pursued than any division of the body” (cited in Paoletti, 2006: 294).
Still’s regard for the fascia however, was exceeded only by his devotion to the circulation of the blood, which he believed to be the quintessential requirement for the maintenance of living tissue. Without the blood the fascia would simply harden from a lack of warmth, fluid and nourishment. From a cupping perspective, powerfully drawing the blood to a site of fascial distress fulfills a crucial requirement for fascial rehabilitation.
The role of the fascia was also at the forefront of the work of Ida Rolf (1896–1979), a PhD in biochemistry from Columbia University, who went on to develop Rolfing. In their book The Endless Web, the rolfers Schultz and Feitis (1996: vii) begin their introduction with, “The muscle-bone concept presented in standard anatomical description gives a purely mechanical model of movement. It separates movement into discrete functions, failing to give a picture of the seamless integration seen in a living body. When one part moves, the body as a whole responds. Functionally, the only tissue that can mediate such responsiveness is the connective tissue.”
Many massage therapists as well, notably during the past decade, have embraced palpating the fascia as the principal diagnostic indicator for applying various release techniques to rectify fascial dysfunction. In addition, many acupuncturists cannot help but be interested in learning that a rapidly growing volume of sophisticated scientific research has validated the concept of the fascial system as an unbroken continuum throughout the body. Like the TCM meridian system, it also functions as a “whole body communication system” (Langevan, 2006:1). It is telling that the interest now shown in the fascia has been spearheaded on two fronts. Firstly by manual therapists, who unlike conventional doctors nowadays specialise in diagnosing and treating softtissue syndromes and have remained active in actually “handling” the body, as was par for the clinical course by practitioners of all medical persuasions back before the emergence of biomedicine.
Secondly, there is a fraternity of researchers and scientists who, backed by sophisticated methods and technologies, are now rapidly expanding our knowledge about this hitherto unglamourous tissue. For an excellent overview of the current research and clinical significance of the fascia, I recommend Fascia: The Tensional Network of the Human Body by Schleip, Findlay, Chaitow and Huijing (2012).
Fascia and Chinese medical theory
In recent years, some TCM writers and researchers have shown a substantial interest in relating the workings of the fascia and its pathways with the elongated geography of the Chinese body maps and their associated mechanisms. Reading much of the new literature about the fascia and comparing it to Chinese medical ideas strikes many a chord. In the Ling Shu (Spiritual Pivot), written during the Han dynasty (200 BC-200AD), are a number of tantalising references to “the space between the skin and the flesh”. For example in chapter four, Qi Bo, the Daoist mentor to Huang Di, describes how noxious qi can penetrate “when the pores are open between skin and flesh” (Wu, 1993:19). As a note of explanation, Wu writes, “Pores between the skin and the flesh, zhou li (sic), may have been a technical term which meant not just the normal pores on the skin but an interactive level in the subcutaneous layer which was activated by pressure, heat or needling.” Therefore the Ling Shu and subsequently all other TCM texts discussing the surface (skin) and immediately below, all emphasise the essential role of this external level as a first-line protective screen. Speaking from an osteopathic perspective, Paoletti (2010: xiv) writes, “The fasciae constitute the first defensive barrier against external insults and come into play prior to any kind of mobilisation of the immune system. The fasciae are thus capable of autonomous decision-making. One could even speak of this system as a “peripheral brain”.
Another elaboration on the fundamental interplay between resistance and “foundations between the skin and the flesh” occurs when Huang Di asks, “When man often has disease of the wind, and perverse sweat pours out, what are the symptoms? This time, another mentor, Shao Yu, replies: “The flesh is without firmness. The foundation between the skin and the flesh is sparse. This results in vulnerability to wind disease” (Wu, 1993:161). Yet another quote from Paoletti (2010: 147) gels perfectly, “In fact no disease process can spread until it has overcome the defensiveness capacities of connective tissue. It has been suggested that for disease to spread it must first interfere with the operations within a basal fascial cell structure called “ground substance”.
Helene M. Langevin, a research assistant professor of neurology at the University of Vermont College of Medicine (USA) and licensed acupuncturist, together with Jason Yandow suggest in their essay, Relationship of Acupuncture Points and Meridians to Connective Tissue Planes (2002:257) that, “the network of acupuncture points and meridians can be viewed as a representation of the network formed by interstitial connective tissue”. They also hold the view, based on their experimental findings, that the correlations between the classical meridian pathways and the broad expanses of fascial sheaths, the location of acupuncture points with concentrations of fascia, and even the elicitation of deqi, which she calls “needle grasp” with “cellular changes that propagate along connective tissue planes” all add to an anatomical perspective of acupuncture as well as “suggest a potentially important integrative role for interstitial connective tissue” (abid, 257).
In another essay, “Connective tissue: A bodywide signalling network?”, Langevin (2006: 1) suggests that fascia links what until now were considered to be separate systems in the Cartesian inspired compartmentalised body. She writes, “Paradoxically a more extensive, even global physiological role for connective tissue was suggested over 2000 years ago by the ancient practice of acupuncture. Traditional Chinese medicine is based on the premise that a network of “meridians” exists within the “fat greasy membranes” extending throughout the body and that this network functionally connects all parts of the body with one another” (2006:1). As for the term “fat greasy membranes” she cites her source to be Paul Unschuld examining the Nan Jing (1986). In her estimation, “since connective tissue plays an intimate role in the function of all other tissues, a complex connective tissue network system integrating whole body mechanical forces may coherently influence the function of all other physiological systems. Demonstrating the existence of such a ‘metasystem’ would therefore change our core of physiology.” (2006:2)

Fig 12: Shirley Gabriel working with the cups.
In practice we have found a corollary of sorts by remodeling what we can palpate at the surface with silicone cups. One example has been reshaping and mending the weakened superficial fascia and extensive stretch marks sometimes associated with childbirth or dramatic weight loss. Patients have informed us that in this therapeutic process, they also feel the benefit of not only knitting the surface but also improving the organ functions below. Patients have informed us that in this therapeutic process, they also feel the benefit of not only knitting the surface but also improving the organ functions below. Our conclusion is that mending the superficial fascia affects everything under its influence, including the viscera.
Other acupuncturists are tantalised by the prospect of the fascia being a solid explanation for the benefits of acupuncture. Legge (2010:vix) makes a case that the Chinese, around 2000 years ago in the Ling Shu, in recognising a system of wide spreading subcutaneous channels called jingjin, may well have provided a remarkable early insight into the fascial pathways and their physiological mechanisms. He feels sure that these were considered to be “specific three-dimensional pathways through the musculo-tendinous tissues” (2012:25).
“Langevin describes the recent findings of the interplay of the fascia as the link that Western medicine has been looking for to tie all the former separate working systems into one holistic scheme.”
Maciocia (2012:285) translates the jingjin to be “muscle channels” or as he would even prefer “channel-like muscles”. His description (ibid 2012: 311-313) of their purpose has a striking resonance with what is now understood about the fascia and its inherent relationship with the structural networking of biotensegrity (d). His list is:
- Protects the body from trauma
- Sustains the body in its erect position
- Maintains the integrity of the body by connecting the “100 bones”
- Governs the movement of joints and allows the movement of the body
- Contributes to the integration of the surface of the body with the interior
- They are nourished by the main meridians
- They contribute to the integration and connection among the three yang channels (greater yang, bright yang and lesser yang) and among the three yin channels (greater yin, lesser yin and terminal yin).
Dr Wang Ju–Yi, a senior TCM clinician practising in Beijing, when asked by his student Jason Robertson (2008:13), “Could you provide a basic definition of the term ‘channel’ (jing luo) and to which physical structure do you understand this term to refer in the physical body?” replied: “There are two answers to this question. Narrowly speaking, one might say that the channels are ‘spaces’ (jian xi) in the body. In this definition, the channels are pathways and might be thought of as the spaces within the fibrous connective tissue of the body. In a larger sense, the concept of the channel refers not only to the spaces but also to everything wrapped within them. In this definition, the concept broadens to include not only the spaces within the connective tissues but also the structures (and fluids) held and brought together by these connective tissues. A channel is then like a river in that it includes the riverbanks and also the complexity of life within the water itself held by those banks. In the body, the channels are then groupings of connective tissue that bring together the blood vessels, bones, lymphatic vessels, nerves, tissues, and interstitial fluids within their purview.” Dr Wang’s appraisal of the channels is an extrapolation of modern anatomical descriptions and the physiological bearings of the fascia from his interpretation within the Chinese medical context, and bears a striking resemblance to the wrap-up of the body systems confirmed by research findings about fascia. “Within the water itself” sounds like a poetic way of describing “ground substance”, the cellular activity within the fascia that determines all the essential workings and behaviour of its influence at a basal metabolic level, going through to the lynchpin directions it gives the myriad other operations it determines throughout the entire physiological system. This corresponds with how Langevin (2006) describes the recent findings of the interplay of the fascia as the “link that Western medicine has been looking for to tie all the former separate working systems into one holistic scheme”.
Cupping and fascial rehabilitation
Thirty years ago or more, when I was asked what tissues I thought were directly engaged during cupping, I’d reply something to the effect, “Judging from what we can see and feel, we can suppose that the various layers of the skin and the fat beneath are drawn inside the cup, together with a positive tension exerted on the underlying fascia.” For a physiological flow-on to this anatomical dimension I’d add, “We can presume therefore that the suction effect and the drawing out and elevation of these tissues facilitates an increase of local blood supply to the immediate area, which in turn implies an enhanced metabolic uptake of oxygen and feed of nutrients to those parts. It therefore relaxes and reduces pain due to congestion and contracture”.

Fig 13: Palpating for problem tissue in the hip.
Over the intervening years, these distinctly “modern” ways of interpreting cupping’s action at a basic level led me to become more and more interested in the effect that cupping has on the body. One way of interpreting cupping as an effective therapy is by its drawing capacity to neutralize and reverse the inward-going dynamic of contracture and in lifting and separating constricted tissue fibres. A reference from 1912 is the first I have found that specifically identifies cupping’s connection with the term “fascia”. In Bier’s Treatment by Induced Hypeaemia (Lathan and Crisp (eds) 1912:57) – hyperaemia being an increase of blood flow to an area of local tissue – it is written, “In this method of treatment only those layers superficial to the deep fascia, viz. the skin and superficial fascia, are, by means of the production of a partial vacuum, sucked into the interior of the glass vessel…”
In an interview with the Melbourne osteopath and lecturer Corey Dyer, he pointed out that with no other mechanism to assist healing, solely releasing and aligning the fascial fibres with cupping would be effective for two to three days. However, if an increased blood flow is brought to the capillary rich fascia, inundating the minute vessels, as we can assume happens with the vacuum effect of cupping, aided by warmth, this active combination of stimuli could alter and correct the tissues in a remarkably effective and longer lasting way.
Stefan Becker, a Brisbane chiropractor who has attended our workshop also had this to say: “If the muscles are chronically tight in an area, the muscle contraction could restrict blood vessels, slowing down blood flow, which could thicken the blood through platelet activity. Cupping could draw stagnant blood and toxins through the muscle to restore blood flow in these areas of chronic myospasm. The act of cupping would also bring phagocytic activity to the area thus “cleaning it up”. This explanation could help to account for cupping marks, whereby the suction effect on the vessels and tissues draws old blood and debris to the skin surface. This is the explanation that medical doctors in Russia gave for cupping after surgery, which was a common practice in many hospitals, at least during the final decades of the Soviet Union. Owing to the noted boost in patients’ recovery from extensive (stationary) cupping by nurses soon after surgery, physicians were led to hypothesise that the old shrunken blood cells are osmotically withdrawn through the vessel membrane by the pull of vacuum, thus prompting the immune system to go into overdrive and produce a new batch of juicy strong cells. The result is a systemic health and recovery impetus.

Fig 14: Lifting a cup to further decompress fascia.
As well, I remember almost 20 years ago visiting the Australian Institute of Sport in Canberra, where the physical and massage therapists frequently applied cupping for the rehabilitation of elite athletes. I was informed that on one occasion when an athlete exhibited a black mark after being cupped, a tissue sample was taken and whisked around to a nearby lab, put under a microscope, and the report was that the fibres were stained with old blood. This goes to show that cupping marks have nothing to do with bruises brought about by trauma.
“Gentle contact and very moderate force is required to restore freedom of movement in certain tissues, while others will require firmer contact and relatively strong manipulation in order to wake them up.”
– Paoletti
The value of other fascia-oriented therapies is founded on their ability to correct myofascial disturbances and instability through handson techniques and movement. We contend that cupping by its exclusive ability to draw outwards and support a myriad of positive reactions likely to benefit the fascia supplies the impetus for positive change in a rapid, dynamic and enduring way. One quote from the Rolfers, Schultz and Feitis (1996: ix) sums it up, “Connective tissue is alive in the sense that it responds to stimulus.” We contend that the vacuum created by cupping exerts such a stimulus.
Diagnosis: palpating fascial discord
There may be more subtle ways of discovering fascial discord, but for our level of understanding and present purpose, we have found that the indications can be determined by palpating with a light to moderate pressure throughout the tissue immediately below the skin surface, using the sensitive finger tips and pads either loosely touching each other or evenly spaced with a small gap of say 1-2 mm. Oil should first be applied to the broad region being investigated. Applying a layer of oil to the skin surface facilitates a clearer appreciation of the errant soft tissue and fibre configurations under the surface. When in good order, most tissue structure at the immediate superficial level of the body has a smooth and moving texture. The therapist should adopt a very relaxed and focused intent at the finger pads. A tuina teacher of mine in Taiwan suggested I believe I have an eye at each fingertip.
We have been surprised that in the literature there appears to be little focus on what we have found to readily demonstrate complaints in relation to the hips. Our experience has shown that even with no information to this effect, a simple test demonstrates whether a person suffers in this region. In those instances where a person feels comfortable and free around the hips, the feeling of the tissue is fairly smooth, firm and compact. When there is pain and discomfort, which may have been there for many decades, the general feeling of the area is quite the opposite. The superficial fascia pertaining to the large expanse of the gluteus maximus can contain large elongated masses of cable-like thickening. Deeper pressure applied into the body of this type of discordance will be met with feelings of discomfort. An even nastier type of pain will be felt to the side of the hip, particularly in the vicinity of the greater trochanter. Finely tuned fingertips will note that the tissue feels discordant, like a complex of spiderlike webbing with associated small knots of exquisite pain. Patients will immediately remark about feelings of discomfort at these locations: “That is my main problem,” to put it politely. We also relate thickening and tightness beside the greater trochanter to adhesions proliferating close around the joint capsule that restrict the inability to move freely, like being bound-up with associated heaviness. Patients sometimes describe this feeling around their hips as like being “stuck in concrete”.
Treatment method
Applying any form of cupping instrument to the flesh in the manner it should be applied to get the best results is in my opinion an art. I am unconvinced by those who seek to mechanically measure how much vacuum pressure is within the chamber of a cup by the number of clicks exerted on the trigger of a pump vacuum gun and treating according to a prescription. It will get to be cupping for different health issues according to a checklist of clicks. Proponents argue that this method makes an application more measured, scientific and precise. I disagree.
For me there is a real finesse in applying a cup. As such, diagnosis is paramount and the determination of how much vacuum is required to engender success is a subtle and sensitive measurement best performed by an accomplished operator who can readily adjust the rate of vacuum and fine-tune exactly how much is appropriate. The same is true when applying a flexible silicone cup.
The practitioner, unless using one hand to squeeze both sides of a cup to mould it into an oblong shape and apply it to a narrow margin of soft tissue area, is required to hold the cup with both hands and lift the lower tier with the finger tips at the same time as compressing the top lid with both thumbs.
This is performed while the cup is held just above the skin. The cup is then gently placed on the body. A slight exertion will secure a soft cup, while added strength is exerted on the lift of the base and the compression of the top to produce a strong suction. Any degree of required strength can be readily determined by this method of application. Paoletti (2006:252) in relation to manual osteopathic treatment of the fascia advises, “Gentle contact and very moderate force is required to restore freedom of movement in certain tissues, while others will require firmer contact and relatively strong manipulation in order to ‘wake them up’ (e).
To release and rectify fascia requires a cup to be drawn very, very slowly across the oiled skin surface. The cup needs to be crawled at snail’s pace with a focused and sensitive intent. The degree of suction is dependent on the condition of the patient and the sensitivity of the area being treated. Corey Dyer, an osteopath, remarked, “The difference in the effect between the slow moving and the fast moving cups may lie in the different effects on the vascular network through the fascial bands undergoing treatment. It would be reasonable to assume that the slower cup has more time to create a local vacuum and pull blood through restricted blood vessels thus restoring a more normal vascular flow and drainage at a local level. Without changes in blood flow, healing cannot take place and any changes are short term.”
When performing sliding cupping, the therapist is advised not to massage the oil deep into the skin pores and into the flesh but to smear it on so it serves no purpose other than being a necessary medium to allow the cup to comfortably move over the surface. Rubbing in the oil is a “no-no” in traditional cupping and the same applies in modern cupping. This is because the oil can clog the passage of toxins being drawn to the skin surface. This is not to say that cupping is therefore contraindicated before or after a light oil massage. It is simply to state that it is better to cup over an area that has not been deeply penetrated with oil.
After treatment, the patient should be instructed to take special care and not expose the treated area to cold or wind, heat or dampness, and avoid air conditioning or blow heaters. The area treated must be covered and the skin pores protected. This is an essential safe keeping dictum for traditional cupping that applies equally to all modern practices.
Compare this level of understanding with the practice of some contemporary therapists, jumping on the cupping bandwagon, who think it is in the best interests of their client to apply ice after cupping, or indeed to put ice into a cup and then apply it. Cupping the surface will open a pathway for the coldness of ice to penetrate deeply into the body, to a joint for example to quell inflammation, but it stays there afterwards with diabolical consequences for the future. I can’t help recalling the old French saying that in the wrong hands, progress can go one step forward and two steps backwards.
“Applying any form of cupping instrument to the flesh in the manner it should be applied to get the best results is in my opinion an art.”

Fig 15: Applying the cup.

Fig 16: Taking a muscle or channel into a stretch and sliding a cup back and forth is an exponential gain. Here the leg is positioned according to a traditional Thai massage move to expose Sen Sahatsarangsi (left leg) and Sen Thawari (right leg) and clear blockages, rid excess wind (lom) and strengthen the legs. Alternatively, from an anatomical perspective, releasing tibialis anterior relieves compartment syndrome, and in TCM we are dealing with the Stomach meridian whereby one effect is to clear stagnation and treat abdominal distention.
Cupping, heat & fascia
For at least as far back as the physicians of Greek antiquity, heat, beyond its requirement to produce a vacuum, has been essential to the therapeutic effect of cupping. In his magnum opus compilation of Greek, Roman and Arabian medicine up until the 7th century AD and including his own works, Paulus Aegineta or Paul of Aegina (625-680 AD), the encyclopedist who is also considered to be the last of the great Byzantine physicians, cites many references to cupping “with great heat”. Among these, for ailments of the breast, stomach and back and for the vomiting of bile, the physician Aetius of Amida said, “a cupping instrument when applied with a great heat, is of great service”. For “when pain is occasioned by warm air or flatulence” (being the windy meteorological condition) again “great heat” is required, and in reference to ischiatic disease (an arthritic complaint seated in the hip joint) “cupping instruments may be applied to the hip with much heat”. Paulus also notes that “earache occasioned by cold … may be greatly remedied by applying a cupping instrument previously heated in hot water, and affixed near the ear” (Adams, 1834).
Understandably, Shirley and I were keen to add this element to our work with the silicone cups. We weighed up our options and decided on soaking them in piping hot water, then dried them off with a towel and tested them – with the results getting a thumbs up! A little later it was satisfying to discover the same method given almost 100 years earlier using rubber cups. In A System of Treatment: Volume One, General Medicine and Surgery (eds, Latham and Crisp, 1914:35) it is advised, “When rubber cups are used they should be soaked in water as hot as the hand can bear, and when thoroughly hot and pliable applied to the skin.” We believe that, regardless of the treatment method being performed for a chronic problem, a heated cup enhances the therapeutic benefit and at the same time feels soothing and comforting. In a conversation with Andrew Gallagher, physiotherapist and founder of the Australian School of Therapeutic Massage, he noted that, “the fascia is very responsive to heat” and Klinger (2012:423) in “Temperature effects on the fascia” writes that “heat in the therapeutic range leads to relaxation of many fascial contractures associated with myofascial dysfunction”.
Fascia strengthening liniment
Herbal liniments have been used as a complement to cupping in Chinese, Western and Islamic medical traditions for centuries. By heating the skin surface, opening the pores, releasing contracture and promoting blood flow, cupping is an excellent method to facilitate the uptake of herbal medicine into both superficial and deeper levels of soft tissue. Simply wipe away as much oil as possible after cupping (if used), and massage in an ample amount of liniment. On page 19 is my formula specifically targeting the restoration of the fascia. This liniment is soaked in alcohol and aims to reconstruct and repair the fundamental deficiency syndrome that emerges over time when fascia and muscle tissue are subject to long-term injury and neglect. For further information on these herbs refer to Bensky, Clavey and Stöger, with Gamble (2004).
A personal treatment
When we procured the more satisfactory blue rubber cups in 2007, Shirley and I began experimenting with them and discovered they could be used for a range of disorders more effectively and comfortably than was possible using the traditional glass and flame or the plastic cup vacuum pump method. Our first trial involved applying them to treat the aftermath of a shoulder injury I had sustained five years earlier. While a tear to the right anterior deltoid and the subsequent horror of a frozen shoulder had made an excellent recovery with acupuncture treatment, I was left with the persistent consequences of soft tissue trauma throughout a large spread of surrounding soft tissue, including fascial knotting and tightness throughout my right intercostal region, an affected scapula margin with difficult to release adhesions around the medial border especially, as well as trigger points and deep-seated pain throughout the arm on the affected side.
It was “fortunate” to have such a problem for experimental purposes because we were aware that using glass cups to treat this region was problematic. The rubber cups proved easy and efficient. Although I had received many sessions of massage and practised a variety of stretching moves on a daily basis, I still had fascia tightness and congestion. To our great satisfaction, engaging sliding cupping to treat the superficial fascia above the broad margins of the latissimus dorsi and throughout serratus anterior, terres major and minor and other muscle groups had an immediate benefit, and all these years later I can attest to its lasting effect. Because of the fixed and durable interlocking of these fibrous nodules, we decided to go in hard with the cups and break them apart. It was a satisfying call because I felt this somewhat aggressive approach was required on this chronic condition.
Oil was applied throughout the intercostal region and a single rubber cup was applied with strong suction. As the cup was dragged, rather than comfortably sliding, it would hit each nodule and move over it causing some discomfort, although its effect felt deeply satisfying, even sublime. Examination by palpation followed and indicated that the nodules had been broken apart and dispersed and positive changes to fascia tissue were achieved. Instead of lumpy tissue pockets and coarse adhesions, the tissue felt smooth and even.
As the cup continued to be moved throughout the broad expanse of the target regions, I was also naturally impelled to respond by taking in huge long breaths of air which felt immensely satisfying, sublime, as my rib cage opened up and I was given the opportunity to indulge in the release from restriction for the first time in years. It became apparent during treatment that the tight nodules that had held fast had restricted the orderly spread of surface fascia, which in turn had tightened the range of my lungs to breathe deeply. When I went to mobilise my arm and shoulder following treatment, my range of movement was complete with no pain.
The other problem on which we tested the flexible rubber cups five minutes later was another remnant of the same shoulder girdle injury. Besides pain throughout my arm, I had developed a chronic trigger point above the elbow joint. It was a painful congestion of tissue that had been stubborn to all previous treatment efforts. Shirley went about moving a small rubber cup back and forth over it and within a minute or two it had dissolved. We both thought something special had occurred.
Case: Fascial disorder of the hip
Five years ago, I treated Peter, a powerfully built man in his mid-30s who presented with debilitating chronic hip pain and instability. Until his retirement two years earlier, he had been an elite player in the English international rugby team for 12 years. Unfortunately injuries throughout his career had dealt a heavy toll and his hips were in a bad way, despite having received the best that sports medicine had to offer. He even explained how he was scared to walk in the park for fear that his hips would “give way” and he would be unable to get up. His main symptoms were throughout his right hip, although he had lesser issues with the other. Palpatory examination had me realise that his was the worst case of fascial discord I had felt in practice. I set to work using flexible cups to see what changes and improvement to his condition might be possible.
Palpation to his right hip, starting from the sacrum and moving laterally below the curved line of the iliac crest, revealed a sequence of thick indurated tissue that felt like my fingers were going over the gauges of a railway track. Further lateral, the entire region surrounding the greater trochanter was tight with a proliferation of matted and lumpy fascia. In the side-lying position, this same fascial disarray continued and lying prone all the tissue indicated similar disorder, taking into account that the palpable characteristics of tensor fascia latae are naturally lumpier than most other fascia surfaces. For the first three treatments I had him lying prone; the following three I had him side lying, and as I was required to go overseas, Shirley continued his treatment rectifying his problems in a supine position. His 10th and final treatment concentrated on any issues he still felt on his left hip. I will now briefly describe Peter’s first treatment. Even during and immediately after his first session, he said his discomfort and confidence with movement had greatly improved.
My first strategy was to release both sides of the Bladder meridian (erector spinae muscles or part of the posterior line in “anatomy trains”) from the shoulders leading down to the sacrum. Maciocia (2012: 308) relates this margin also to the Bladder muscle channel, which influences both gluteus maximus and gluteus medius.

Fig 17: Cups left on the hip to release deeper levels than possible by sliding cups, as well as attracting the therapeutic profit obtained by sliding along and freeing the Gall Bladder/lateral line.
Second, I applied four stationary cups to his left hip at the following locations: Juliao (GB 29), Huantiao (GB30), Yaoyan (Extra point) and above the site of gluteus medius, and left them active for 20 minutes. I knew from an acupuncture perspective that treating the opposite side would not only benefit the local site but would also transfer a deep release to the right side I was rectifying with sliding cups. During this time I went about applying the fascial release methods with sliding cups to his right hip.
Palpation revealed that his fascia below the iliac crest was very indurated, with wavelike elevations bunched tightly in bands approximately 1.5cm wide, while either side of each tight elevation, approximately 2cm across, the fascia was loose and frayed. As I moved the cup very, very slowly across this dire discord, I had my first experience of feeling the quivering from the tissue conducted into my hand. I explained to Peter what was occurring, and as we were getting on well, enquired if he would be fine about me substituting the flexible cup for a glass cup for a short while. I wanted to feel if there was any sense of what was conducted into my hand with a hard-bodied cup. There was none. Fourth, I concentrated on lifting and releasing the fascia around the greater trochanter and any other areas that required attention. A focus also was pressing into these margins and drawing the cup by lifting away from the concentrations of what I took to be adhesions between muscle sheaths as well as connections to the bone, to allow a return to normal biomechanics. The soft tissue engaging the greater trochanter belongs to the pathway of the Gallbladder muscle channel (Macioca, 2012:287), and besides travelling along the sides of the body, also has a wide divergent branch that runs to the sacrum influencing gluteus maximus and gluteus medius, and another pathway that spreads anteriorly to influence tensor fascia latae.
I then released the stationary cups from his left side and used a heated towel to warm the whole area and get rid of any residual oil from the right hip before I gently massaged in an ample quantity of heated fascia strengthening liniment. Fifth, I began some preliminary sliding cupping very slowly down his Bladder (postero-lateral surface) and Gallbladder (middle lateral) channels softening and releasing an abundance of indurated tissue throughout both margins.
After treatment I re-examined the entire region and the change to the tissue was dramatic. Peter got up from the table and said his hips felt the best they had for a decade, and with each ongoing treatment the result was an improvement to the entire region. Progress mounted after each treatment without any hint of setback. I contacted Peter only a week ago to ask if the work had maintained its benefit. He replied “Yes.”
Chiropractor Stefan Becker had this to say about corrugations or indurations in the upper hips: “Adhesions form and tighten and contract between folds of fascia. I can see this happening anywhere in the body. Collagen is laid down in any area where there is damage followed by resultant healing, so these areas of retracted fascia could form anywhere there has been damage. I see cupping exerting an influence on indurations at the surface, breaking down adhesions between the folds of fascia. The result: fascia and muscle sheaths are no longer contracted, which enables the muscles to pull evenly and cleanly.”
A final note
It is still early days for this subject and practice, and the bulk of what has been presented is a summary. We look forward to further research on this complex topic. What should encourage our confidence is the fact that we are dealing with phenomena of substance. We are engaging with the stuff of the natural world, and therefore success should be forth-coming. In the meantime, the immediate practical benefits of this treatment remain in the hands of practitioners.
My thanks to Shirley Gabriel and also to Corey Dyer and Stefan Becker for their fascial illuminations and “bravo” to all cited researchers and writers. Got a comment or something to share? Please contact me at healthtr@iinet.net.au.
Footnotes
- (a) My plural references henceforth refer to colleague Shirley Gabriel, to whom I owe my thanks for her many contributions to the development of Modern Cupping.
- (b) Readers may be interested to know that I have contributed a chapter to the coming third edition of Ilkay Chirali’s book Chinese Cupping Therapy with an essay called “Cupping’s folk heritage: people in practice.”
- (c) For a detailed description of “sha” refer to the essay “Gua Sha: Gently Scraping Out the Sha” (Bentley, 2007).
- (d) For an excellent introduction to biotensegrity see Levin and Martin in Schleip, Findlay, Chaitow and Huijing (2012).
- (e) Please read “Cupping Deficiency” (Bentley, 2010) for a description of appropriate vacuum levels for different health and soft tissue conditions.
Bibliography
- Adams, Francis (1834) The Medical Works of Paulus Aegineta. Vol. 1. J.Welsh: Treuttel, Wurtz, & Co: London.
- Bensky, D., Clavey, S. and Stöger, E. with Gamble, A. (2004) Chinese Herbal Medicine: Materia Medica. 3rd Edition. Eastland Press: USA.
- Bentley, Bruce (1996) Cupping as Therapeutic Technology. Master of Arts (in Health Studies) thesis. Latrobe University, Melbourne.
- Bentley, Bruce (2007) Gua Sha: Smoothly Scraping Out the Sha. The Lantern. Vol. 4, No. 2. Can be read at www.healthtraditons.com.au Bentley, Bruce (2011) Cupping Deficiency. The Lantern: Vol 8, No. 2. Can be read at www. healthtraditons.com.au.
- Christpoulou-Aletra, Helen and Papavramidou, Niki (2008) Cupping: An Alternative Surgical Procedure Used by Hippocratic Physicians. The Journal of Alternative and Complimentary Medicine. Vol. 14 No. 8. Mary Ann Liebert Inc.
- Davis, Audrey and Appel, Toby (1979) Bloodletting Instruments in the National Museum of History and Technology. Smithsonian Studies in History and Technology No 46. Smithsonian Institution Press: Washington.
- Eliade, Mircea (1989) Shamanism: Archaic Techniques of Ecstasy (translated by Willard R. Trask). Arkana. Penguin Books: Great Britain.
- Elkin, A.P. (1994) Aboriginal Men of High Degree: Initiation and Sorcery in the World’s Oldest Tradition. Inner Traditions: USA.
- Grant, Edward. (Ed.) (1974) A Source Book in Medieval Science. Harvard University Press. Cambridge. Jones, W.H.S. (1967) Hippocrates Vol. IV. William Heinmann Ltd: Great Britain
- Klinger, Werner (2012) “Temperature effects on the fascia” in Schleip, Findlay, Chaitlow and Huijing, Fascia: The Tensional Network of the Body. Churchill Livingstone Elsevier: China.
- Langevin, Helene M. and Yandow, Jason A. (2002) Relationship of Acupuncture Points and Meridians to Connective Tissue Planes. The Anatomical Record (New Anat). Wiley-Liss, Inc. Langevin, Helene M. (2006) Connective tissue: A body-wide signaling network? Elsevier. Accessed online at http://elsevierhealth.com/journals/mehy August 2010.
- Langevin, Helene M. and Huijing, Peter A. (2009) Communicating About Fascia: History, Pitfalls, and Recommendations. International Journal Therapeutic Massage & Bodywork. 2(4): 3–8. Published online 2009 December 7.
- Latham, Arthur and English, T. Crisp (eds) (1912) A System of Treatment: By Many Authors. Volume III. Special Subjects. J. & A. Churchill: London.
- Latham, Arthur and English, T. Crisp (eds) (1914) A System of Treatment, in Four Volumes. Volume I, General Medicine and Surgery. The MacMillan Book Company: Great Britain.
- Legge, David (2010) Jinjin: Acupuncture treatment of the muscular system using the meridian sinews. Sydney College Press: Hong Kong.
- Levin, Stephen M. and Martin Danièle-Claude (2012) Biotensegrity: Mechanics of Fascia in Schleip, Robert. Findley, Thomas W. Chaitow, Leon and Huijing, Peter A. Fascia: The Tensional Network of the Human Body. Churchill Livingstone Elsevier: China.
- Maciocia, Giovanni (2012) The Channels of Acupuncture: Clinical Use of the Secondary Channels and Eight Extraordinary Vessels. Churchill Livingstone Elsevier: China.
- Myers, Thomas (2009) Anatomy Trains: Myofascial Meridians for Manuel and Movement Therapists. Churchill Livingstone Elsevier: China.
- Myers, Thomas (2010) Discovery Through Dissection: The Anatomy Trains Perspective. Massage & Bodywork. January/February.
- Paoletti, Serge (2006) The Fasciae: Anatomy, Dysfunction & Treatment. Eastland Press: China.
- Potter, Paul (1995) Hippocrates Volume VIII. Harvard University Press. Cambridge, MA.
- Schleip, Robert. Findley, Thomas W. Chaitow, Leon and Huijing, Peter A. (2012) Fascia: The Tensional Network of the Human Body. Churchill Livingstone Elsevier: China.
- Schultz, R. Louis and Feitis, Rosemary (1996) The Endless Web: Fascial Anatomy and Physical Reality. North Atlantic Books: Canada.
- Smith, Wesley D. Hippocrates VII. Harvard University Press. Cambridge, MA.
- Thomas Stratton (1853) Proposal to Substitute an Elastic Cup for the Present Cupping-Glass. The Lancet. Volume 2. Ed by Thomas Wakely. George Churchill: London.
- Underwood, E. Ashworth (1955) Bleeding, Cupping, and Purging, in British Medical Journal. Jan 1. Paul Unschuld (1986) Nan-ching: the classic of difficult issues: with commentaries by Chinese and Japanese authors from the third through to the 20th century. University of California Press: Berkley.
- Wang Ju-Yi and Jason D. Robertson (2008) Applied Channel Theory in Chinese Medcine: Wang Ju-Yi’s Lectures on Channel Therapeutics. Eastland Press: Seattle.
- Wickkiser, Bronwyn L. (2008) Asklepios, Medicine, and the Politics of Healing in Fifth Century Greece: Between Craft and Cult. The John Hopkins University Press: USA.
- Withington, E.T. (1968) Hippocrates Vol.111. The University Press: Great Britain.
- Wu, Jing-Nuan (2007) Ling Shu or The Spiritual Pivot. Asian Spirituality, Taoist Studies Series. USA.
Pictorial credits
- FIG 1: Batty, Philip, Allen Lindy and Morton, John eds. (2005) The Photographs of Baldwin Spencer. Museum Victoria.
- FIGS 2 & 3: Phillips, E.D. (1973) Aspects of Greek Culture. The Charles Press. United States of America.
- FIG 4: Tiemann, George & Co., (1889) American Armamentarium Chirurgicum, SI photo 76-13542 Figure 1653 New York.
- FIG 5: Evans and Wormull (1893) Illustrated Catalogue of Surgical Instruments, Apparatus and Appliances, manufactured by Evans and Wormull. William Clowes. London.
- FIGS 6, 7, 11, 12, 13, 14, 15: Photographs by the author.
- FIGS 8, 9 & 10 Photographs by Alan Sinclair.
- FIG 15, 16: Photographs by Michael Ellis.
- FIG 17: Photography by Danuta Stone.
Fascia liniment
- Ài Yè (Artemisiae Argyi Folium) – warm, dispels cold dampness, stops pain due to cold.
- Dù Zhòng (Eucommiae Cortex) – warm, strengthens the sinews especially the lower back and knees, aids smooth flow of qi and blood, (with esp. Dú Huó).
- Chuān Xiōng (Chuanxiong Rhizoma) – warm, moves the blood and promotes the qi, disperses blood stasis.
- Niú Xī (Chuanxiong Rhizoma) – neutral, disperses blood stasis, strengthens sinews and bones.
- Ròu Guì (Cinnamomi Cortex) – hot, warms and tonifies yang, disperses deep cold and warms the channels.
- Xù Duàn (Dipsaci Radix) – sl. warm, promotes movement of blood alleviates pain and reconnects sinews and bones. Literal English translation: “reconnect what is broken”.
- Gān Jiāng (Zingiberis Rhizoma) – hot, unblocks channels, revives yang and expels cold. Disperses cold qi in all channels.
- Guì Zhī (Cinnamomi Ramulus) – warm, releases the muscle layer, unblocks yang qi, releases the exterior, warms and unblocks the channels and collaterals: for wind-cold-damp obstruction, expels wind.
- Dú Huó (Angelicae Pubescentis Radix) – warm, dispels wind, dampness and cold especially the lower back and legs, for acute and chronic disorders, tracks down lurking wind.
- Qiāng Huó (Notopterygii Rhizoma Seu Radix) – warm, effective for dispelling wind with a focus on the upper and more superficial aspects of the body.
Bruce Bentley studied Chinese medicine in Taiwan from 1976 until 1981. He has a Masters Degree in Health Studies based on his thesis entitled Cupping as Therapeutic Technology. He has investigated the Eastern tradition of cupping in Vietnam, and studied at the Shanghai University of Traditional Chinese Medicine, the Tibetan Medicine Hospital in Lhasa, Tibet, and at the Uighur Traditional Medicine Hospital in Urumqi, Xinjiang Provence, China. To research the Western practice of cupping, Bruce visited the Australian Institute of Sport in Canberra where masseurs employ cupping to treat injuries and enhance performance, and in 1998 he went to Europe and North Africa, doing archival research on cupping at the Wellcome Institute for the History of Medicine, London, and the Department for the History of Medicine at Rome University, followed by field-work in Sicily, Greece, Bulgaria, Turkey, Morocco and Tunisia learning local cupping traditions. Bruce’s most recent research trip investigating cupping was in Cambodia during July 2003. He is also a state registered acupuncturist and Chinese herbalist and director of Health Traditions: www.healthtraditions.com.au.
Top ↑
